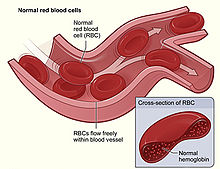
Anemia (also spelled anaemia in British English) is a blood disorder in which the blood has a reduced ability to carry oxygen. This can be due to a lower than normal number of red blood cells, a reduction in the amount of hemoglobin available for oxygen transport, or abnormalities in hemoglobin that impair its function. The name is derived from Ancient Greek ἀν- (an-) 'not' and αἷμα (haima) 'blood'.
When anemia comes on slowly, the symptoms are often vague, such as tiredness, weakness, shortness of breath, headaches, and a reduced ability to exercise. When anemia is acute, symptoms may include confusion, feeling like one is going to pass out, loss of consciousness, and increased thirst. Anemia must be significant before a person becomes noticeably pale. Additional symptoms may occur depending on the underlying cause. Anemia can be temporary or long term and can range from mild to severe.
Anemia can be caused by blood loss, decreased red blood cell production, and increased red blood cell breakdown. Causes of blood loss include bleeding due to inflammation of the stomach or intestines, bleeding from surgery, serious injury, or blood donation. Causes of decreased production include iron deficiency, folate deficiency, vitamin B12 deficiency, thalassemia and a number of bone marrow tumors. Causes of increased breakdown include genetic disorders such as sickle cell anemia, infections such as malaria, and certain autoimmune diseases like autoimmune hemolytic anemia.

Anemia can also be classified based on the size of the red blood cells and amount of hemoglobin in each cell. If the cells are small, it is called microcytic anemia; if they are large, it is called macrocytic anemia; and if they are normal sized, it is called normocytic anemia. The diagnosis of anemia in men is based on a hemoglobin of less than 130 to 140 g/L (13 to 14 g/dL); in women, it is less than 120 to 130 g/L (12 to 13 g/dL). Further testing is then required to determine the cause.
Treatment depends on the specific cause. Certain groups of individuals, such as pregnant women, can benefit from the use of iron pills for prevention. Dietary supplementation, without determining the specific cause, is not recommended. The use of blood transfusions is typically based on a person's signs and symptoms. In those without symptoms, they are not recommended unless hemoglobin levels are less than 60 to 80 g/L (6 to 8 g/dL). These recommendations may also apply to some people with acute bleeding. Erythropoiesis-stimulating agents are only recommended in those with severe anemia.
Anemia is the most common blood disorder, affecting about a fifth to a third of the global population. Iron-deficiency anemia is the most common cause of anemia worldwide, and affects nearly one billion people. In 2013, anemia due to iron deficiency resulted in about 183,000 deaths – down from 213,000 deaths in 1990. This condition is most prevalent in children with also an above average prevalence in elderly and women of reproductive age (especially during pregnancy). Anemia is one of the six WHO global nutrition targets for 2025 and for diet-related global targets endorsed by World Health Assembly in 2012 and 2013. Efforts to reach global targets contribute to reaching Sustainable Development Goals (SDGs), with anemia as one of the targets in SDG 2 for achieving zero world hunger.
Signs and symptoms


A person with anemia may not have any symptoms, depending on the underlying cause, and no symptoms may be noticed, as the anemia is initially mild, and then the symptoms become worse as the anemia worsens. A patient with anemia may report feeling tired, weak, decreased ability to concentrate, and sometimes shortness of breath on exertion. These symptoms are unspecific and none of the symptoms alone or in combination show a good predictive value for the presence of anemia in non-clinical patients.

Symptoms of anemia can come on quickly or slowly. Early on there may be few or no symptoms. If the anemia continues slowly (chronic), the body may adapt and compensate for this change. In this case, no symptoms may appear until the anemia becomes more severe. Symptoms can include feeling tired, weak, dizziness, headaches, intolerance to physical exertion, shortness of breath, difficulty concentrating, irregular or rapid heartbeat, cold hands and feet, cold intolerance, pale or yellow skin, poor appetite, easy bruising and bleeding, and muscle weakness.
Anemia that develops quickly, often, has more severe symptoms, including, feeling faint, chest pain, sweating, increased thirst, and confusion. There may be also additional symptoms depending on the underlying cause.
In more severe anemia, the body may compensate for the lack of oxygen-carrying capability of the blood by increasing cardiac output. The person may have symptoms related to this, such as palpitations, angina (if pre-existing heart disease is present), intermittent claudication of the legs, and symptoms of heart failure.
On examination, the signs exhibited may include pallor (pale skin, mucosa, conjunctiva and nail beds), but this is not a reliable sign.
Iron-deficiency anemia may give symptoms that can include spoon-shaped nails, restless legs syndrome, and pica (the medical condition indicates the desire for things that are not food, such as ice, dirt, etc.). A blue coloration of the sclera may be noticed in some cases of iron-deficiency anemia. Vitamin B12 deficiency anemia may result in decreased ability to think, memory loss, confusion, personality or mood changes, depression, difficulty walking, blurred vision, and irreversible nerve damage.Other specific causes of anemia may have signs and/or complications such as, jaundice with the rapid break down of red blood cells as with hemolytic anemia, bone abnormalities with thalassemia major, or leg ulcers as seen in sickle cell disease.
Causes
The causes of anemia may be classified as impaired red blood cell (RBC) production, increased RBC destruction (hemolytic anemia), blood loss and fluid overload (hypervolemia). Several of these may interplay to cause anemia. The most common cause of anemia is blood loss, but this usually does not cause any lasting symptoms unless a relatively impaired RBC production develops, in turn, most commonly by iron deficiency.
Impaired production
- Disturbance of proliferation and differentiation of stem cells
- Pure red cell aplasia
- Aplastic anemia[35] affects all kinds of blood cells. Fanconi anemia is a hereditary disorder or defect featuring aplastic anemia and various other abnormalities.
- Anemia of kidney failure due to insufficient production of the hormone erythropoietin
- Anemia of endocrine disease
- Disturbance of proliferation and maturation of erythroblasts
- Pernicious anemia is a form of megaloblastic anemia due to vitamin B12 deficiency dependent on impaired absorption of vitamin B12. Lack of dietary B12 causes non-pernicious megaloblastic anemia.
- Anemia of folate deficiency, as with vitamin B12, causes megaloblastic anemia
- Anemia of prematurity, by diminished erythropoietin response to declining hematocrit levels, combined with blood loss from laboratory testing, generally occurs in premature infants at two to six weeks of age.
- Iron-deficiency anemia, resulting in deficient heme synthesis
- Thalassemias, causing deficient globin synthesis
- Congenital dyserythropoietic anemias, causing ineffective erythropoiesis
- Anemia of kidney failure (also causing stem cell dysfunction)
- Other mechanisms of impaired RBC production
- Myelophthisic anemia or myelophthisis is a severe type of anemia resulting from the replacement of bone marrow by other materials, such as malignant tumors, fibrosis, or granulomas.
- Myelodysplastic syndrome
- anemia of chronic inflammation
- Leukoerythroblastic anemia is caused by space-occupying lesions in the bone marrow that prevent normal production of blood cells.
Increased destruction
Anemias of increased red blood cell destruction are generally classified as hemolytic anemias. These types generally feature jaundice, and elevated levels of lactate dehydrogenase
- Intrinsic (intracorpuscular) abnormalities cause premature destruction. All of these, except paroxysmal nocturnal hemoglobinuria, are hereditary genetic disorders.
- Hereditary spherocytosis is a hereditary defect that results in defects in the RBC cell membrane, causing the erythrocytes to be sequestered and destroyed by the spleen.
- Hereditary elliptocytosis is another defect in membrane skeleton proteins.
- Abetalipoproteinemia, causing defects in membrane lipids
- Enzyme deficiencies
- Pyruvate kinase and hexokinase deficiencies, causing defect glycolysis
- Glucose-6-phosphate dehydrogenase deficiency and glutathione synthetase deficiency, causing increased oxidative stress
- Hemoglobinopathies
- Sickle cell anemia
- Hemoglobinopathies causing unstable hemoglobins
- Paroxysmal nocturnal hemoglobinuria
- Extrinsic (extracorpuscular) abnormalities
- Antibody-mediated
- Warm autoimmune hemolytic anemia is caused by autoimmune attack against red blood cells, primarily by IgG. It is the most common of the autoimmune hemolytic diseases. It can be idiopathic, that is, without any known cause, drug-associated or secondary to another disease such as systemic lupus erythematosus, or a malignancy, such as chronic lymphocytic leukemia.
- Cold agglutinin hemolytic anemia is primarily mediated by IgM. It can be idiopathic or result from an underlying condition.
- Rh disease, one of the causes of hemolytic disease of the newborn
- Transfusion reaction to blood transfusions
- Mechanical trauma to red blood cells
- Microangiopathic hemolytic anemias, including thrombotic thrombocytopenic purpura and disseminated intravascular coagulation
- Infections, including malaria
- Heart surgery
- Haemodialysis
- (e.g. angiodysplasia)
- Gynecologic disturbances, also generally causing chronic blood loss
- From menstruation, mostly among young women or older women who have fibroids
- Antibody-mediated
- Parasitic
- Trypanosoma congolense alters the surfaces of RBCs of its host and this may explain T. c. induced anemia
- Anemia of prematurity, from frequent blood sampling for laboratory testing, combined with insufficient RBC production
- Trauma or surgery, causing acute blood loss
- Gastrointestinal tract lesions, causing either acute bleeds (e.g. variceal lesions, peptic ulcers, hemorrhoids) or chronic blood loss
- any type of cancers, including colorectal cancer and cancer of the urinary bladder, may cause acute or chronic blood loss, especially at advanced stages
Diagnosis

Peripheral blood smear microscopy of a patient with iron-deficiency anemia 
A Giemsa-stained blood film from a person with iron-deficiency anemia. This person also had hemoglobin Kenya. Definitions
There are a number of definitions of anemia; reviews provide comparison and contrast of them. A strict but broad definition is an absolute decrease in red blood cell mass, however, a broader definition is a lowered ability of the blood to carry oxygen. An operational definition is a decrease in whole-blood hemoglobin concentration of more than 2 standard deviations below the mean of an age- and sex-matched reference range.
It is difficult to directly measure RBC mass, so the hematocrit (amount of RBCs) or the hemoglobin (Hb) in the blood are often used instead to indirectly estimate the value. Hematocrit; however, is concentration dependent and is therefore not completely accurate. For example, during pregnancy a woman's RBC mass is normal but because of an increase in blood volume the hemoglobin and hematocrit are diluted and thus decreased. Another example would be bleeding where the RBC mass would decrease but the concentrations of hemoglobin and hematocrit initially remains normal until fluids shift from other areas of the body to the intravascular space.
Testing
Anemia is typically diagnosed on a complete blood count. Apart from reporting the number of red blood cells and the hemoglobin level, the automatic counters also measure the size of the red blood cells by flow cytometry, which is an important tool in distinguishing between the causes of anemia. Examination of a stained blood smear using a microscope can also be helpful, and it is sometimes a necessity in regions of the world where automated analysis is less accessible.
| Age or gender group | Hb threshold (g/dL) | Hb threshold (mmol/L) |
|---|---|---|
| Children (0.5–5.0 yrs) | 11.0 | 6.8 |
| Children (5–12 yrs) | 11.5 | 7.1 |
| Teens (12–15 yrs) | 12.0 | 7.4 |
| Women, non-pregnant (>15yrs) | 12.0 | 7.4 |
| Women, pregnant | 11.0 | 6.8 |
| Men (>15yrs) | 13.0 | 8.1 |

